| Outbreak: Foundation Farm Raw Milk | |
|---|---|
| Product: Foundation Farm Raw Milk | Investigation Start Date: 04/10/2012 |
| Location: Clackamas, Multnomah and Washington Counties, Oregon | Etiology: E. coli (STEC) O157:H7 |
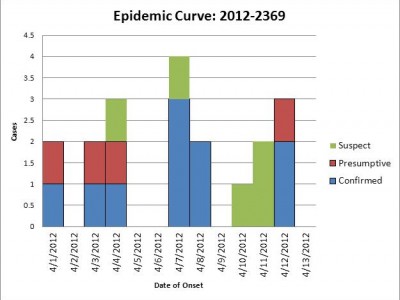
| Earliest known case onset date: 04/01/2012 | Latest case onset date: 04/14/2012 |
| Confirmed / Presumptive Case Counts: 11 / 5 | Positive Samples (Food / Environmental): 2 / 13 |
| Hospitalizations: 4 | Deaths: 0 |
This outbreak highlighted the persistent hazard of raw milk consumption, already well documented in the medical literature. Four of the 11 cases were hospitalized — some critically ill and all with hemolytic-uremic syndrome (HUS), subsequently shown to have been caused by E. coli O157:H7. Although most sales of raw milk are illegal in Oregon, the farm implicated here is an example of one method by which those determined to get the product can skirt the law: instead of “purchasing milk,” families bought “shares” in Foundation Farm cows, their dividends being the milk produced by them and then consumed without pasteurization.
The cause of the outbreak wasn’t long a mystery: Oregon local public health nurses routinely interview each O157 case and ask about “usual suspect” exposures — one of which is whether the case consumed unpasteurized milk. A single case having a high-risk exposure like this one is sufficient to raise suspicion and to warrant further investigation. As the investigation progressed, it transpired that the families that participated in this “cow-share” arrangement had already been aware of many illnesses and communicating among themselves about them; and the dairy farmer had therefore advised the shareholders not to drink the milk. The farm ceased production, and several parents publicly advised the unwary not to serve unpurified milk to their children.
On April 10, 2012, the Multnomah County Health Department was notified by a clinician about a 1 year-old child with HUS (culture pending; later shown to be O157:H7). The child attended a day-care center in Washington County and had a history of regular raw milk consumption, both of which indicated a need for public health follow-up.
Washington County public health officials investigated the child-care facility and identified no other suspected cases there. Meanwhile, Oregon Health Authority (OHA) officials conferred with those from the Oregon Department of Agriculture (ODA) to discuss action that could be taken regarding the herd-share operation that was reportedly the source of the raw milk. It was determined that the operation (dba Foundation Farm), although unlicensed and unknown to Agriculture officials, had been operating legally, with 4 cows, 3 of which were in production. (Dairies of this type are not required to be licensed or regulated in Oregon.) ODA officials contacted the farm owner to request a list of its customers so that they could be contacted and asked about potential illness.
On the morning of April 11th, the farmer reported to ODA that, in the course of contacting his customers through Facebook, he had learned of several additional illnesses. He also reported that he had voluntarily stopped distribution of milk and had recommended to his customers that they discard any available product. Upon request, he sent a list of the 48 household contacts for his customers, and authorized ODA to visit the premises and to collect specimens from the working part of the farm.
That afternoon, while local and state public health officials commenced case finding among herd-share households, OHA investigators and an ODA official visited the dairy farm. They collected 63 samples including rectal swabs on all 4 dairy cows, surfaces in and around the milking parlor, and fecal pat samples from adjacent pastures. No milk was available at the farm for testing.
Over the ensuing days, OHA investigators attempted to interview all households on the list using a standardized questionnaire regarding history of Foundation Farm milk consumption, several other possible food exposures, and diarrheal illness in household members.
(CONTINUED BELOW ↵)
A press release was issued to warn the public about the risk and to stimulate reporting. One of the earliest identified cases was from a household that was not on the customer list: that child had consumed the milk while visiting a family friend.
Leftover raw milk samples were collected for testing on April 12 and 13 from two shareholder households.
Results:
Ultimately, 11 lab-confirmed cases—including 1 Washington State resident who consumed the milk while visiting family in Oregon—and 5 presumptive cases were identified. Four other household members reported very mild concurrent diarrheal symptoms and were not counted as cases. Four cases were hospitalized—all with HUS. Three cases were hospitalized for >25 days. Representatives of 30 (62%) of the 48 herd-share households, comprising 91 individuals, were interviewed. All 16 cases had consumed FF milk on one or (usually) multiple occasions. No other suggestive common exposures were identified.
The farm setup was described by ODA as fairly typical for a family farm. The layout was poorly designed from a food-safety perspective. The premises appeared to be difficult to maintain in a hygienic manner for food production. There were no facilities for rapid chilling of milk. Milk bottles were reportedly stored in an ordinary (non-commercial) refrigerator.
Culture of 13 (21%) of 63 samples collected at Foundation Farm yielded E. coli O157:H7; positive samples included 10 of animal manure, 2 cattle rectal swabs and 1 swab of fencing at the milking station. One of two milk samples collected from customer households was also positive. All but one of the O157 strains isolated from cases, milk, and the farm were indistinguishable by 2-enzyme pulsed-field gel electrophoresis (PFGE); 1 case appeared to have an extra band with XbaI digestion.
Conclusions:
This outbreak was caused by consumption of unpasteurized contaminated milk. Consumers should be warned that, without a kill step such as pasteurization, there is no reliable way to render milk free of harmful microbes. In particular, E. coli O157 infection can cause bloody diarrhea, hemolytic uremic syndrome and even death.