| Outbreak: Cal-Farms Parsley | |
|---|---|
| Product: Parsley | Investigation Start Date: 10/20/2005 |
| Location: Deschutes County, OR | Etiology: E. coli (STEC) O157:H7 |
| Earliest known case onset date: 10/08/2005 | Latest case onset date: 10/27/2005 |
| Confirmed / Presumptive Case Counts: 3 / 61 | Positive Samples (Environmental / Water) 10 / 2 |
This 2005 McGrath’s Fish House outbreak of E. coli O157:H7 infections was traced back to parsley from Cal-Farms. The journey to finding the source was interesting: 206 people interviewed, 64 ill people, extremely muddy field conditions, cattle near the flooded parsley fields, and even evidence of heavy deer presence.
Background
On October 20, 2005 we were notified of two E. coli O157:H7 cases from two adjacent counties, Deschutes and Jefferson. Routine follow-up interviews revealed that both ate at a popular restaurant in Bend on the same day, October 12, 2005. Seeing this as a possible common-source exposure, the Deschutes County Health Department in Bend attempted active case finding by obtaining the names of restaurant patrons who used credit cards on October 12th. An initial quick survey identified several other diners who reported gastrointestinal symptoms after their meal. A formal case-control study was launched using an expanded list of credit card names from October 12-15, and a questionnaire based on restaurant menu as well as characterization of illness, if any.
Methods
Names from the credit card list were used to look up telephone numbers on the Internet. Deschutes County staff and MPH students from the Acute and Communicable Disease Program (ACDP) of the Oregon Department of Health Services interviewed people. Several people reported gastrointestinal illness after eating at the restaurant. On October 23, 2005, the Deschutes County Health Department decided to issue a press release. Medical alerts were sent to the local physicians and emergency rooms. The press release stimulated additional reports of illness. E. coli O157:H7 isolates were subtyped by pulse-field gel electrophoresis (PFGE) People who reported GI illness were asked to submit stool specimen for confirmation. Some gave specimens to the local health department, while others gave specimens to their doctors.
Environmental Inspection
The Deschutes County Environmental Health section inspected the restaurant. Employees were asked about recent GI illness. Environmental samples and food samples were collected.
We visited Cal-Farms in Oregon City, reviewed their operations, and obtained parsley sales records for September and October. We were shown 2 fields that were the source of parsley harvested in September and October, and collected ~100 convenience samples of soil and parsley stubble on November 7th from both fields. There were no obvious deficiencies in operating conditions to these inexpert observers. Several potential sources of O157 were noted, including livestock in nearby fields (goats, lamas), river water used for irrigation (in drier months), and a deer presence heavy enough to merit repellent next to parsley fields. Because extremely muddy conditions made it difficult to seal sample bags, these were pooled into 6 composite samples – 3 from each field. These samples were enriched and tested by multiplex PCR and cultured on CT-SMAC for O157 at the Institute for Environmental Health (Lake Forest Park, WA; courtesy Dr. Masour Samadpour).
Results
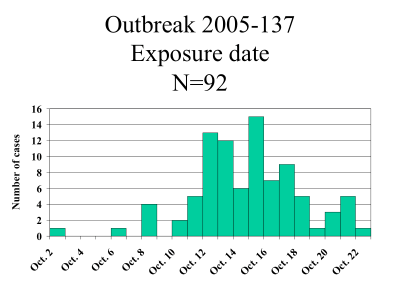
A total of 206 people were interviewed, including people who called in after the press release was issued. Of 120 completed interviews derived from the credit card names, 33 (27%) reported GI illness, of whom 23 (19%) met a working case definition (three or more loose stools in a 24 hour period, and incubation period > 1 day and < 10 days). In total, we identified 64 people who reported three or more loose stools (Figure 1). The median incubation period was 2.6 days. Forty-three (67%) were females, and the median age was 51 (range 4-87). Meal dates for those who were ill were from October 2 – October 22 (Figure 2).
Symptom profile is shown on Table 1. Twenty-one people reported having bloody diarrhea, and only 7 (33%) of these sought medical care. Of those who sought medical care, 6 (86%) were asked to give stool specimen.
| Symptoms | Number | % |
|---|---|---|
| Diarrhea | 64 | 100% |
| Cramps | 51 | 80% |
| Nausea | 33 | 52% |
| Headache | 26 | 41% |
| Myalgia | 19 | 30% |
| Bloody diarrhea | 17 | 27% |
| Vomiting | 13 | 20% |
| Fever | 8 | 13% |
By our initial univariate analysis, crab and artichoke dip, coconut prawns, and vegetables were all significantly associated with illness, but none of these items accounted for more than 20% of the cases.
As we were considering these results, first-enzyme PFGE results on the initial isolate were posted to PulsNet revealing a match to a recently investigated cluster (2 restaurant groups, and 2 sporadic cases) in Washington. Washington epidemiologists had identified parsley (traced to an Oregon supplier and grower) as the likely vehicle for those cases. Armed with this knowledge, we then considered parsley as a potential vehicle for the McGrath’s outbreak. We determined that parsley from the same supplier (Pacific Coast Fruit) and farm (Cal-Farms, Oregon City) had been the sole source of parsley at McGrath’s from XX through ~ October 10 (last delivery date on October 10th). Parsley was used on a large number of menu items, including several side dishes that unfortunately had been omitted from the questionnaire. We reanalyzed our data, using a composite variable standing in for all the food items served with parsley. Limiting the analysis to meal dates from October 12-15 and adding abdominal cramps to the case definition, we found parsley to be significantly associated with illness (OR=3.32, p-value = 0.02). This variable could explain about 80% of the cases. Other food items that were significant included vegetables (OR=3.18, p-value = 0.02) and red potatoes (OR=4.44, p-value = 0.03), both of which had parsley. Interestingly, we learned that the crab and artichoke dip was always served with parsley-topped bruchetta.
Food samples and environmental samples tested negative at the Oregon State Public Health Laboratory (OSPHL). Water and the filter from the ice machine were tested, and were negative.
| Parsley | Case | Control | Total |
|---|---|---|---|
| Yes | 24 | 41 | 65 |
| No | 6 | 34 | 40 |
| (Total) | 30 | 75 | 105 |
| OR = 3.32 | 95% CI = 1.11-10.39 | P-value = 0.028 |
| Vegetables | Case | Control | Total |
|---|---|---|---|
| Yes | 12 | 13 | 25 |
| No | 18 | 62 | 80 |
| (Total) | 30 | 75 | 105 |
| OR = 3.18 | 95% CI = 1.11-9.18 | P-value = 0.027 |
| Red Potatoes | Case | Control | Total |
|---|---|---|---|
| Yes | 6 | 4 | 10 |
| No | 24 | 71 | 95 |
| (Total) | 30 | 75 | 105 |
| OR = 4.44 | 95% CI = 0.98-21.10 | P-value = 0.03 |
Discussion
Parsley from Cal-Farms was the apparent cause of the McGrath’s outbreak, by extension, all recent Oregon and Washington cases with matching PFGE. The only food item that explained most of the cases was the parsley. The fact that the three confirmed cases matched the Washington cluster suggest a common source. Seven of the 8 cases in Washington had foods that had parsley, and the parsley came from the same grower. The Washington cases had other things in common, such as romaine lettuce, roma tomatoes, red cabbage, and onions, but these food items came from different distributors.
The parsley farm distribute to various places including grocery stores. Pacific Coast Fruit, the distributor for the restaurant, is only one of a number of their customers. It is not clear why this distributor would get a contaminated batch and why only a few restaurants would get contaminated parsley. This wholesaler got about 28% of the sales from 9/1/05 – 10/28/05.
We would have expected to see a lot more cases since the parsley was distributed to other places too.
During the visit to the farm, a number of possible sources of contamination were noted. There were deer repellents, and deer tracts. Samples of parsley and dirt were tested, but were negative.
Only 3 cases were confirmed out of 64 ill people. Five additional cases were tested, but no E. coli O157 were detected. The specimens were collected 9-15 days after onset of diarrhea. Most adults do not excrete the organism after ~2 weeks, and 3 weeks in kids. Three cases were tested through their private physicians, and
were negative. Interestingly, most cases did not seek medical care, even those with bloody diarrhea. Of those with bloody diarrhea, 33% sought care, and of these, 86% were cultured.
The restaurant voluntarily closed on October 24th and was cleaned thoroughly. All the food workers were tested and were negative. The restaurant was reopened on November 1st. We did not hear of new cases after the restaurant was reopened.
The recommendations were:
1) Throw out all left over foods.
2) Emphasize employee hand washing.
3) Ill employees should not work until symptoms resolve, or if they are culture positive for E. coli O157, they should have 2 negative stools before returning to work.